STI research in Ganjoni, Mombasa
As a result of the mortality resulting from the HIV-AIDS epidemic, even researchers have not paid much attention to other STI’s outside of HIV research.
‘It is very hard to get data on STI’s in Kenya except for certain groups like HIV infected or on high risk groups like commercial sex workers. For some of the diseases, we don’t have the capability to test for,’ said Dr Linnet Masese, a PhD student at the University of Washington and a clinician at the Ganjoni Municipal Communicable Disease Control Centre, commonly referred to as the Ganjoni Clinic.
In the wake of newspaper reports of increasing use of the morning after pill and young women soliciting abortions, there is a dire need for information on the other consequences of unsafe sex.
‘Young women worry about pregnancy but there can be far worse outcomes that will result in a life of anguish. Women often bear the brunt of the consequences of untreated STI’s,’said Dr Masese.
The most common STI’s are chlamydia, gonorrhea, Trichomaniasis, genital herpes and syphilis among others. The World Health Organization (WHO) estimates that between 333-448 million new cases of curable STI’s occur yearly in the world.
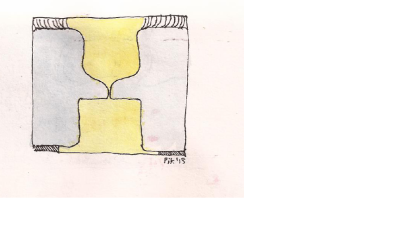
One of the commonest direct complication of untreated STI is pelvic inflammatory disease (PID) in women. PID occurs when STI’s invade the fallopian tubes and uterus. When STI’s invade the fallopian tubes, they may cause scarring which blocks the egg from moving down the tube. The sperm cannot get to egg and as a result there is no fertilization. Such a woman cannot conceive. According to the WHO, 30 to 40 percent of female infertility is as a result of PID.
STI’s may also partially block the fallopian tube which will allow the sperm to get to the egg and fertilize it, but the fertilized egg remains stuck in the tubes and develops as though it were in the uterus. This is known as an ectopic pregnancy. It can rupture and cause internal bleeding, even death. WHO statistics state that 40 to 50 percent of ectopic pregnancies are as a result of PID.
Scarring of the reproductive organs may also cause chronic pelvic pain that lasts months or years.
‘The tragedy with STI is that most infected people, do not experience any signs of illness. While these infections silently continue to damage their reproductive organs, these people are also spreading the infection to others,’ said Dr Masese
Out of every 10 people infected with an STI, 9 to 7 will not experience any symptoms. The 1to 3 out of 10 that are lucky to experience clinical signs or symptoms may be prompted to seek treatment. However, these few may be afraid to seek treatment in government clinics due to the stigma associated with STI infection. Many people believe that STI’s are diseases of the sexually promiscuous. Although it is true that a person with many partners or one whose partner is promiscuous, have more chances for exposure to STI’s, it is not always the case.
According to Dr Scott McClelland, associate professor at the University of Washington and visiting lecturer at the University of Nairobi, who has spent many years conducting research on STI at the Ganjoni clinic in Mombasa, some women can be unlucky.
‘Chlamydia is a very common infection within the population and it is a disease of young people. The first boyfriend a girl has may pass a Chlamydia infection on to her. She may have only that one partner, yet the Chlamydia will remain in her, causing damage to her reproductive organs and when she is ready to have children, she finds that she is infertile,’ said Dr Scott.
The other reason that someone with symptoms of STI may resist seeking treatment is the fear that the government facility may ask them to present their partner for treatment as well.
‘Although partner notification and treatment is not mandated in Kenya, the thought of being asked by the clinician to bring one’s partner is enough to deter people from seeking treatment at government hospitals. Another deterrent is exposing one’s private parts to a clinician, especially if the clinician is young,’ said Dr Masese.
Most people suffering from STI will therefore seek care in pharmacies where partner treatment is not offered and where treatments may not be adequate. In the end, the STI’s continue to spread within the community and damage the fertility of many young women unnecessarily.
In addition to their impact on fertility, STI’s have been shown to increase one’s risk of acquiring and transmitting HIV. Research conducted by Dr Scott among others at the Ganjoni clinic has contributed convincing evidence that the present of STI’s including rarely talked about Trichomonas infection, increases the risks of acquiring HIV. Studies conducted at Ganjoni have also shown that provision of ART to HIV positive commercial sex workers does not lead to an increase in risky sexual behaviour.
For vaccine development, Ganjoni clinic has contributed data that has send scientists back to the drawing board. The data showed that women infected with one strain of HIV can still be infected with another stain of the virus. This situation, called superinfection, demonstrated that a vaccine that mimicked natural infection would not be effective in preventing HIV acquisition.
Research on STI’s in Ganjoni clinic begun in 1993. This clinic enrols women that are involved in transactional sex to participate in studies related to STI and HIV. In 1993, only HIV negative women were recruited into the studies which looked at risk factors for acquiring HIV. These women visited the clinic on a monthly bases and were treated for STI, provided with free condoms and taught how to use them. When ARV’s became available, all those who tested HIV positive and met certain immunity criteria according to Kenyan guidelines, were put on treatment. In 2000, the clinic started recruitment of HIV positive women into studies that continue to explore various aspects of STI among HIV infected women.
Away from the scientific output, one exciting outcome is the drop in HIV acquisition among this group of women. In 1993, out of every 100 women recruited at the start of the year, 15 would be HIV positive at the end of the year. Twenty years on, only 1 out of every 100 HIV negative women recruited will be positive at the end of the year. The results of marked reduction of HIV infection among this high risk population has been replicated across the country from the early studies in Pumwani and Majengo women in Nairobi.
Although these dramatic reductions in HIV infections in this group of women who are at high risk of getting infected with and spreading HIV have been noted in research settings, it is possible to replicate this in a cheaper way. Currently there are Sex worker outpatient (SWOP) clinics in Nairobi among other places. Such centres can be replicate across the country and work to keep the level of STI low in the community.
For such centres to succeed, outreach is needed to recruit participants, women are encouraged to get a HIV test, all STI are treated, free condoms are provided and women taught how to use them. HIV negative women are encouraged to maintain their status by treating all STI and using condoms while HIV positive women are put on treatment. Research has shown that transmission of HIV among those on ART is minimal
However, adolescent girls require attention. In countries like America, Chlamydia had been identified as a risk for infertility and so the country targets schools for testing and treating this STI. For this to happen, research needed to be conducted in these young girls to establish the presence of Chlamydia. The testing is not invasive as it requires a urine sample, but it may be difficult to do in Kenya.
‘First and foremost we don’t have data on Chlamydia among our young people. But it’s a difficult study to do as we need parental consent to conduct these studies. It is not an easy thing to do STI research on young people as we are a society unwilling to accept that our young girls are sexually active,’ said Dr Masese.
Unless we know how much Chlamydia is in the population, we will not be able to provide the services that are needed to reduce its impact on fertility. Unfortunately, tests for Chlamydia are expensive, so it is difficult to diagnose. There is urgent need for simple, cheap, easy to use tests, similar to a pregnancy test, to diagnose STI’s like Chlamydia.
Chlamydia being a disease of the young will require a more innovative approach to protect against its impact. Currently all HIV and STI prevention campaigns focus on the use of the latex male condom. Consistent and correct use of which will reduce the giving or getting of STI. But the surest way to avoid infection is to abstain from vaginal, anal, and oral sex, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
Without this, testing and treatment of STI is the best way forward. However, there are lessons to be learned from HIV, the most famous STI. According to the 2007 Kenya AIDS Indicator Survey (KAIS) conducted in a country wide sample of 15, 853 men and women aged 15-64, out of every 10 HIV positive people in Kenya, only 2 were aware of their status. Considering that millions of shillings have been spent drumming the ‘know your HIV status’ message, it is uncanny, that 8 out of 10 HIV positive Kenyans are unaware of their status. However, the campaigns have enabled a great reduction in the stigma associated with HIV. There appears to be more stigma attached to STI’s than HIV so if we are to have increased testing and awareness of all STI, a more creative approach is required.