
Antibiotic resistance – it’s no small matter.
My mother once had a tenant whose child’s breath smelt of paracetamol syrup…. and. it was not a one off thing. I was on a visit home one day when the child was taken to local clinic by the mother who returned home with a bag of drugs. I asked her what the child was suffering from and this is the answer I got…..
‘Daktari alisema mtoto ana kapneumonia kidogo na tumalaria kidogo’
That translates roughly to the doctor said the child had a little bit of pneumonia and a little bit of malaria.
I don’t claim to be a doctor, but this child did not have a fever, was breathing OK, but had a runny nose. Malaria is not a common disease in central Kenya and what was this ‘little pneumonia’?
Yet the child was given antimalarials, antibiotics and of course, paracetamol syrup.
This misuse of antibiotics leads to the development of antibiotic resistant bacteria. Infections caused by antibiotic resistant bacteria take longer to treat and cause unnecessary deaths. According to the WHO, drug-resistant bacteria are estimated to cause 25,000 deaths in the European Union alone and to cost governments US$ 1.5 billion every year. It is no simple matter.
That is why the UN general assembly currently meeting in New York, yesterday asked member countries to commit to fighting antimicrobial resistance (AMR).
Allow me to make a simple statement here – microbes are bacteria, viruses, fungi and parasites. The most misused antimicrobials are antibiotics that are used to fight bacterial infections.
I was lucky to be working at the Kenya Medical Research Institute in Kilifi and so anytime my children felt unwell, I took them to the staff clinic which only dispensed drugs when the blood results showed they were needed. When my kids said they were unwell, I knew for sure they were not trying to skip school because they always got a blood test any time they had a fever. Although they spend between 7 – 10 years in Kilifi, which is a malaria endemic area, my children were never treated for malaria, because none of their blood results showed malaria parasites. They also rarely got antibiotics.
However, even though I knew the clinicians were right, there were times I wished for drugs just to feel that I was doing something for my sick child. But as a scientist, I trusted their judgement and sure enough, a day or two of rest at home with plenty of fluids, favourite food and TV was all they needed for the body to fight of whatever was affecting them.
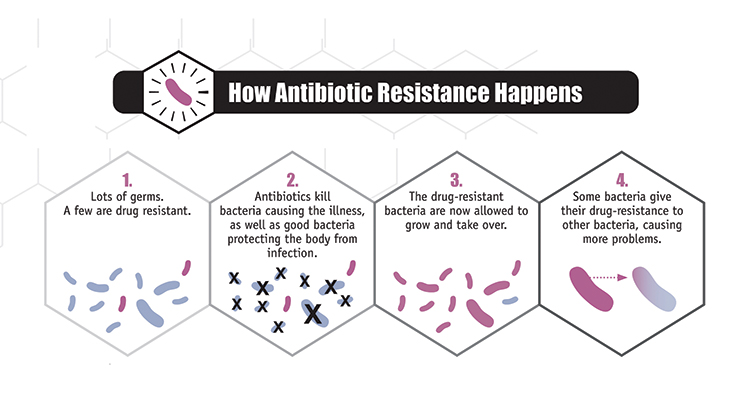
Thing is, the very use of antibiotics leads to resistance as this diagram illustrates
Naturally, over time, a change will occur in the DNA of bacteria that enables them to survive in the presence of an antibiotic. These mutant bacteria will not spread quickly if bacteria sensitive to the antibiotic remain the majority. But if there is constant antibiotic use, the sensitive bacteria are cleared and the resistant bacteria given a chance to become dominant. This process can be slowed down significantly if antibiotic use is restricted.
A lot of time people think they are the ones resistant to drugs. It is not an individual, it is being infected by bacteria that are resistant to drugs.
In Kenya, many health practitioners, especially in private practise, want to prescribe more drugs for more sales. The patients who are paying for the service also want to feel that the doctor is doing something, so they also want drugs for their children.
I do understand where mothers and careers are coming from. Children under the age of 5 get ill very frequently. Their body is for the first time making contact with new bacteria and virus within their environment. They frequently have fevers and runny noses. Don’t get me wrong, each bad cough and fever ought to be investigated, but if it is clear that it is not a lower respiratory tract infection, then as careers, we should be content and not insist on unnecessary treatments. If you live in an area where malaria is not common, and the tests are negative, do not insist on buying antimalarials over the counter.
Like my mother’s tenant, there are children all over the world smelling of paracetamol, drinking antibiotics by the litre, for absolutely no purpose. In Kenya, most of these antibiotics are prescribed by a health professional.
It’s not just among children but adults as well. There is tendency to use drugs until one feels better and then just stop before the dose is complete. This gives bacteria an opportunity to reproduce with low levels of the drug, which then accelerates the generation of drug resistant bacteria.
Health professionals have a duty not to overprescribe: to appease parents or make more sales. It is a minor gain when you consider that long term, there will be no drugs to make money from as microbes develop resistance to the drugs available and patients begin to doubt that you are any good.
Antibiotic use in animals is also part of the problem and I will discuss this next time.
Comment
Comments are closed.


MARY
Great article- and also the issue of not adhering/complying to the antibiotics once they have been rightfully prescribed …is another contributing factor.