How PCV fared in the UK – lessons learnt
This week, I shall be sharing light on issues regarding the Pneumococcal Conjugate Vaccine(PCV) – the vaccine that our children currently receive to reduce pneumonia and meningitis as a result of pneumonia bacteria.
I start of with results from other countries that introduced the vaccine earlier and see how us in East Africa can learn from them.
By the end of this week – you shall know everything, well, a lot, about PCV.
Scientists made the first vaccine that contained 7(out of the 90) of the most vicious serotypes and called the vaccine Pneumococcal Conjugate Vaccine-7 (PCV7). This vaccine was first introduced in USA and other countries who had the money to pay for it.
One of those countries was the UK, which introduced PCV-7 in September 2006. Surveillance was essential to monitor whether disease was going down and whether the nasty serotypes for which the vaccine offered protection were replaced by milder pneumococcus bacteria that were sometimes equally vicious, when the space was freed for them.
Unlike the Kenyan PCVIS(Pneunococcal Conjugate Vaccine Impact Study) which relied on a total of just over 250,000 people in a demographic surveillance system in Kilifi, England and Wales have a good vital registration system. Hospital data is all computerised and so it is possible to collate data for all the children admitted in any hospital in the country.
Their equivalent of PCVIS covered the full population of England and Wales, a total of 54.8 million people.
Since all hospital data in the UK is computerised, it was possible to know what each child admitted to any hospital had suffered from and track changes in Invasive Pneumococcal Disease (IPD).
A little reminder of what IPD is…
Pneumococcal bacteria are normal residents in the back of the noses of humans but occasionally, these bacteria invade the body causing Invasive Pneumococcal disease (IPD). This manifests as pneumonia or meningitis, a very serious infection of the covering of the brain and spinal cord. Those most at risk of IPD are the elderly and children under five especially those with weak immune systems.
Back to the study……
Scientists compared data in the pre-vaccination period 2001 – Sept 2006 to data post introduction of PCV-7 Sept 2006 to 2010.
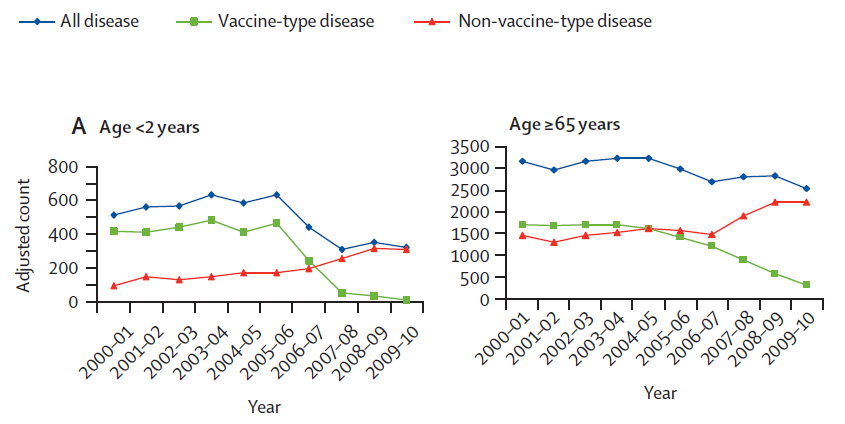
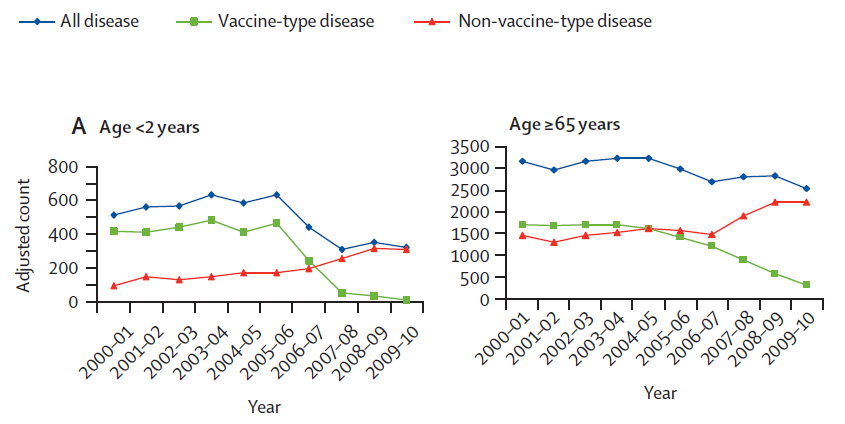
This study was published in The Lancet journal by Prof Elizabeth Miller of the Health Protection Agency in the UK in 2011. Prof Miller and colleagues looked at the age specific trends in IPD in all ages. I have chosen to focus on children under 2 years of age and adults over 65 years of age. The data and graphs for those 2-64years of age are available in The Lancet paper.
Why have I picked these two age groups?
The youngest children have the weakest immune systems and are therefore most at risk of invasive disease
But why adults over 65 years of age?
As you can imagine younger children visit their grandparents and leave them with whatever bacteria they have been spewing from their noses. Elderly people have a poor immune system and easily succumb to IPD from the bacteria left behind by their grandchildren. Scientists in the USA found that introduction of PCV-7 led to a reduction in IPD in those over 65 years of age. Vaccinating children was shown to provide protection against IPD in the elderly. This protection by proxy is known as herd immunity.
I picked out these two graphs that looked at how disease changed with the introduction of PCV-7 in England and Wales as reported by Prof Miller and colleagues.
Let’s examine each line, bearing in mind that PCV-7 was introduced in England and Wales in September 2006.
The green line
Disease as a result of the serotypes for which the vaccine offered protection – known as vaccine type – was greatly reduced after the introduction of PCV-7. Both in children under 2 who were vaccinated and those over 65 years of age who though not vaccinated also showed a steady drop from 2006. Prof Miller and colleagues showed that the IPD from the 7 serotypes for which the vaccine offered protection, decreased by 98% in children 2 years and under and by 81% for those over 65.
Fairly impressive – everyone would long for a vaccine that works this well. Almost total protection for those vaccinated and then additional protection for those people who are around them- nothing could be better.
But alas!
The red line
Let’s look at the red line…..scroll back and have a look.
The red line shows disease as a result of serotypes that were not included in PCV-7. IPD from those serotypes for which the vaccine did not offer protection (non vaccine type), went up. Non-vaccine type disease increased by 68% in children under 2 and by 48% in those over 65 years of age. IPD caused by replacement serotypes is known as serotype replacement disease. It is the reason why surveillance is so crucial after introduction of PCV.
The blue line
The blue line shows how IPD as a whole dropped within these two age groups. The overall effect of the vaccine was ruined by the non-vaccine types coming in. Among the elderly, the effect of this non vaccine type disease was so high as to greatly reduce the impact of removal of the serotypes for which the vaccine offered protection. The overall reduction of IPD in those over 65 years was only 19% when you took account of disease from the non-vaccine serotypes.
For children under 2, despite the non-vaccine bacteria taking the place of the vaccine type there was still an over 50% reduction in IPD in this younger age group.
As a result of the impact of serotype replacement disease, England and Wales switched to PCV-13 in 2010. While PCV-7 offers protection against 7 serotypes of pneumococcal bacteria, PCV-13 offers protection against 13 serotypes which include most of the important serotype replacement ones. With PCV-13, the immune system was primed to recognise more of the invasive types of bacteria.
Without surveillance, it would have been difficult to work out what was happening after the introduction of PCV-7 and the effect of serotype replacement disease would have been missed.
The point of surveillance and vigilance cannot be over-emphasised as put rather neatly by lead researcher in Kilifi, Prof Anthony Scot.
‘The overall point is that unlike ‘Diphtheria’ where we introduced the vaccine and forgot about the disease, controlling pneumococcal disease will require both surveillance and vigilance – to select the right vaccine and to know when to introduce it. This is the function of the EPI program manager and his team – to keep a tab on the disease and optimise the investment in (expensive) vaccines,’ said Prof Scott.
I will write more about how introduction of PCV-13 in England and Wales is doing next time.
Comment
Comments are closed.


Mary
Very informative!