Dying babies – part II
Last week, I raised the issue of babies dying at birth and it reminded me of a visit I made to a facility in Kenya in 2014.
This mother told me how she had laboured a day and a night at a dispensary in the rural area, over 10 km from the county hospital. The nurses at that dispensary had been very helpful and the mother had not a single bad word to say about them. They had rung the county hospital, which was the referral hospital, to bring out an ambulance so that the mother would deliver in the safety of the hospital. But because it had rained, the ambulance driver was not allowed to come through the mud. An NGO Landcruiser that was passing through the area, took the mother to the county hospital – by then it was 2 days after labor begun, the child had been born asphyxiated in a dispensary that had no oxygen. It was a desperate situation, the damage was done and the options were that the baby would die or that he would survive severely impaired and would require his mother for the rest of his life. It was heartbreaking. The baby died on his second night in the hospital.
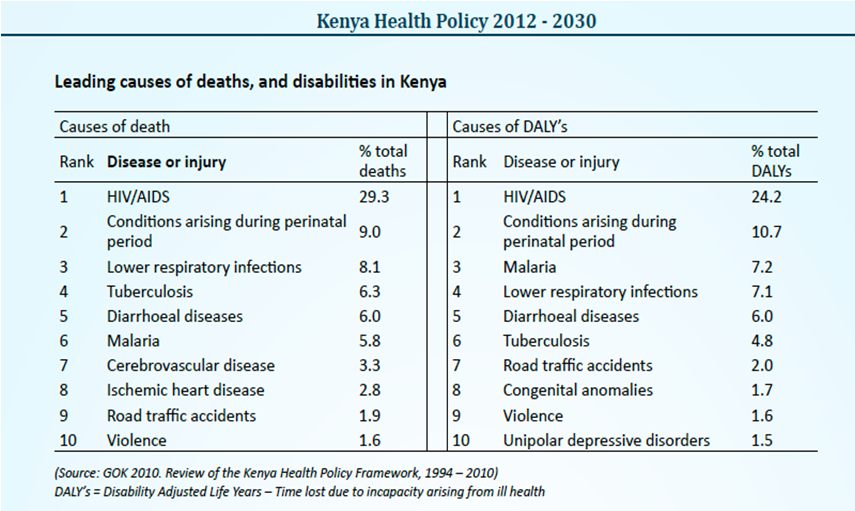
In the year 2009, there were 42,013 neonatal deaths in Kenya. The first 28 days of life are referred to as the neonatal period and a child under a month old is a neonate. The data suggests that 60 % of all children that die before the age of one, die within the first 28 days of life.
Dr Jalemba Aluvaala of KEMRI-WTRP in Nairobi, conducted a large study in 22 hospitals in Kenya which all had a neonatal unit and each delivered about 300 babies a month. In a paper Dr Aluvaala published in 2014 in the journal, Archives of Childhood Diseases – the most common cause of admission for neonates was birth asphyxia. The data showed that 36% (over 7 out of every 20 admissions) were a result of birth asphyxia. Of 1,249 admissions, there were 166 deaths, 60% of which occurred within the first day of admission.
Birth asphyxia, is lack of oxygen that occurs during birth.
If detected early in the delivery process, babies can be born healthy through speedy intervention – for example by a quick CS or forceps delivery. Babies with mild asphyxia at birth are given breathing support until they can breathe well enough on their own, and then are closely monitored. Hospitals and dispensaries need to have a reliable oxygen supply for this to happen. Oxygen was available in the hospitals that Dr Aluvaala and colleagues did their study.
Babies with more serious asphyxia may need mechanical ventilation (a breathing machine), respiratory therapy, fluid and medicine to control blood pressure and prevent seizures. Doctors may need to delay feedings to give the baby’s bowel time to recover.
The length of time the child fails to get enough oxygen determines the damage caused to the child. However, there is always that child, who despite the best of care, passes away as a result of birth asphyxia or deteriorates faster than usual and suffers the impacts despite the best of care.
Most common and severe disability as a result of birth asphyxia is cerebral palsy. Others include, epilepsy and learning problems later in life.
With the increase in babies born in hospitals, there is added pressure on neonatal facilities where they exist. Most dispensaries are like the one in the example I described above, rarely have oxygen. Mother and baby have to wait and be taken to the referral hospital, at which point, the child is severely ill. The mother will then go home either with a severely disabled child that will remain in this child-like form and need her care for the rest of the his/her life or with a body to bury.
This mother will not get the support she needs to cater for her child. I have written about the state of children with disability before…..
A clinician who has practiced for over 20 years in many parts of the world, said this to me.
‘I feel particularly that governments need to be made aware that reducing mortality is great, understanding the millennium goals is great, achieving them is great but you need to look at the expense. What is the expense? There is the push to reduce child mortality but there is no effort into dealing with children with neurodisability. Where is physiotherapy to support them? These children become a social burden’.
You may or may not be raising a severely disabled child. You may or may not understand the weight of taking care of a baby that will never dress or feed themselves, a child you can never hold a conversation with, who will never call you ‘mum’. But you can put yourself in this mother’s shoe.
If we are going to push for a reduction in child mortality – we must face up to the fact that it comes hand in hand with an increase – temporarily – of neurodisability. We must address issues of how to take care of these children, not leave them to the mother alone.
Of course, it need not lead to more neurodisability if rural dispensaries have the right equipments and training to handle neonates. According Dr Jalemba Aluvaala – health care workers in Kenya do not receive much formal instruction on the care of neonates and all they learn is from placements during their internships.
Ensuring that health practitioners in the dispensaries are well trained, have the equipment they need and enough staff to handle the burden of work is crucial. Otherwise we shall continue to scapegoat individuals while disability rises.